- Menu
- Home
- Consultation
- Cosmetic Surgery
- Cosmetic Surgery
- Anti-Aging
- Infosheets
- Tariffs
- FAQs
- BOOK A CONSULTATION
Book a Consultation

Infosheets
Click on + below for more information.
Definition and foreword
Abdominal skin and fat excess often alters self confidence. Liposuction has improved dramatically the outcome of abdominal aesthetic surgery, by reducing the amount and the length of scars.
There are different types of abdominoplasty depending on the patient's examination. The following parameters will influence the surgeon's final decision: skin quality, amount of fat tissue, abdominal muscle tonicity and the overall patient's morphology.
Usually, there are two groups of patients : one requirering isolated liposuction and another requirering abominoplasty. The aim of this procedure is to remove the impaired abdominal skin (stretched skin, scars, stretch-marks) and tighten the remaining surrounding skin. Localised fat excess can be removed during the same procedure by liposuction and impared abdominal wall muscles may be treated too (widening, herniae).
The standard abdominoplasty (Tummy Tuck) removes a large amount of redundant tissue (skin and fat) from the middle and lower abdominal wall, between the belly button (umbilicus) and the pubic region, according to preoperative planning. The healthy skin from the upper middle part of the abdomen is then redraped downwards in order to replace the removed impaired skin. The belly button is preserved and put in its normal position through a hole cut and countoured in the newly draped skin. This procedure leaves a scar. It's length and position may vary with the amount and location of skin to be removed. It usually extends from above the pubic hair to the groin region. Its length is determined in preoperative planning and the patient shall be fully aware of it.
Isolated abdominal liposuction
See Liposuction.
Before the operation
- A preoperative check-up is made according to your surgeon's recommendations.
- The anaesthesiologist will be seen in consultation at latest, 48 hours prior to surgery.
- No medication containing aspirin will be taken for 10 days before surgery.
Type of anesthesia and hospital stay duration
Type of anesthesia
Abdominoplasty is usually performed under general anaesthesia. The patient is asleep through the entire operation.
Hospital stay
The duration of hospital stay is usually 2 to 5 days.
The procedure
Every surgeon has his or her personal technical habits which he or she adapts to every new case, in order to obtain the best possible results. However, there are common principles:
The position of the skin incisions, which will correspond to the future scars, depends on the amount of skin to be removed. The more skin there is to remove, the longer the remaining scars.
The excessive fat is aspirated with liposuction and the stretched abdominal wall muscles are tightened.
A molding dressing is made at the end of the procedure. Depending on your surgeon and the extent of fat and skin tissue necessary to remove, the operation takes about 90 minutes to 3 hours.
After the operation
It is recommended to wear a pressure garment for 2 to 4 weeks, day and night. You shall not go to work for 2 to 4 weeks. The scars are often red during the first 2 or 3 months and progressively become paler starting from the third month onwards, during a period of 1 to 3 years. The scars should be protected from sunlight and UV for at least 3 months. Sporting activities can be progressively started after 6 weeks.
The result
It can be best appreciated one year after the procedure: During this period, it is recommended to be patient while scars slowly fade, and collaborate with your physician for a regular follow-up consultation every 3 months during one year. Concerning scars, you should know that they do fade away with time but never completely disappear. The surgeon does the sawing, but scarring is a patient-related process. However, abdominoplasty offers an often noticeable aesthetic improvement. It enhances the patient's comfort, quality of life and self confidence, thus helping him or her to reach for a better weight-control.
Imperfect results
Most of the time, a properly indicated abdominoplasty can offer a real improvement to patients in terms of satisfying results and conformity to their expectations.
In some cases, localized imperfections can be observed, which must be distinguished from genuine complications: -The scar can be a bit too visible, adherent or asymmetric. It can sometimes become widened, hypertrophic or bumpy (cheloid). -The belly button may look unnatural. -In some case, when there is excessive tension on the scar, the pubic hair can be raised upwards.
These problems can be corrected secondarily under local anaesthesia after 6 months.
Possible complications
Abdominoplasty, even if performed for aesthetic reasons, is a genuine surgical procedure, with the consequent risks related to all medical acts, no matter how mild they might appear. There are surgical and aesthetic complications.
Concerning anaesthesia, the anaesthesiologist will inform you about all the anaesthetic risks. You must be aware that anaesthesia can sometimes cause unpredictable body reactions that can be difficult to control. The presence of an experienced anaesthesiologist, in a surgical environment, means that the risks are statistically practically negligible.
In fact, techniques, products and monitoring methods have progressed considerably over the last twenty years, offering optimal safety, especially when the operation is elective and the patient is in good general health.
Concerning surgery: by choosing a competent and qualified Plastic Surgeon, experienced in performing this procedure, you limit, but do not entirely eliminate, surgical risks.
Indeed, some complications can occur after abdominoplasty which constitutes one of the heaviest procedures in Plastic and Aesthetic Surgery.
Among possible complications, you must be aware of the following:
- Thrombo-embolic accidents (blood clot in the veins of the legs, pulmonary embolism) are rare, but can be life-threatening. They can be prevented by strict prophylactic measures, such as standing and walking as soon as possible after surgery, wearing compression stockings, or heparin therapy (low doses of heparin injected under the skin)
- Blood clots (haematomas) are quite rare but can occur. They can be evacuated to prevent an impairment of the final aesthetic result.
- Infection, though uncommon, can be treated with drainage and antibiotics.
- It is common to notice 8 days after surgery a lymph collection accumulating under the skin. Such a collection can be drained and will dry up rapidly without sequela.
- Localised skin necrosis. Large areas of necrosis is rare. They can be prevented by a proper preoperative examination and a cautious and well-executed operation, with moderate tension on sutures.
- Numbness of abdominal skin may be observed, frequently in the lower parts of the abdominal wall. It is usually transient and most patients recover normal feeling after 3 to 12 months.
- In some patients with very damaged skin or skin with poor circulation, the healing process may be delayed.
General conclusion about plastic and aesthetic surgery of the abdominal wall
Plastic and aesthetic surgery of the abdominal wall has made dramatic progress. There are techniques and strategies (isolated liposuction, mini or plain abdominoplasties) which can solve most of the aesthetic problems encountered in the abdominal area.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
The movement as well as the iterative lose of weight are "demanding" a lot to the skin of the inner part of the arm. It's why the number of skin ptosis ( not amenable to an isolated aspiration ) is higher than the simple fat hypertrophies. When skin distension takes place at this level, a lipoaspiration alone can't be sufficient and just a skin tightening can improve this deficiency. This is what we call the arm lifting or the arm inner part lifting. The aim of the surgery is to take away the excess of skin, to decrease the underneath fat infiltration and to redistribute the skin.
Before the operation
A meticulous clinical examination will determine the more appropriate type of surgical procedure, you need (choice of incision, associated lipoaspiration indicated or not). At the time of the first consultation, a precise information on the different surgical steps, on the follow-up and the expected results will be given to you. Specially, where the scar will be taken place will be well explained.
- A usual pre-operative evaluation is done, following the prescriptions.
- An anesthesiologist must be seen in consultation, at least 48 hours before surgery, in case of general anaesthetic or "vigil" one.
- No medicine with aspirin in it must be taken for at least 10 days before surgery.
- Depending on the type of anesthesiology, it can be asked to you to keep fasting (no food, no beverage) for 6 hours before surgery.
Type of anesthesia and hospital stay duration
Type of anesthesia
The inner arm lifting can be done under general anaesthesia, under local anaesthesia completed by tranquillizing drugs, injected in veins ("vigil" anaesthetic) or also, in some cases, under simple local anaesthetic. The choice between these different techniques must come after you have discussed it with the surgeon and the anaesthesiologist.
Hospital stay
The surgery can be done in the "day care" department; it means, you can leave hospital the same day of the surgery, just after a few hours of resting and medical supervision. On the other hand, you may be asked to stay in hospital over the night; it means, you enter the hospital early morning, the day of surgery (or sometimes the day before in the afternoon) and leave it the day after surgery.
The procedure
Each surgeon is using his own technique, he may adapt to each case, in order to get the best result. Different techniques have been described. The fat infitrated the skin is removed by lipoaspiration. The skin excess is removed, what leaves a scar which location and length depend on the amount the skin laxity and on the procedure choosen. The skin incision can be vertical, longitudinal,along the arm inner side or horizontal, following a armpit fold. Sometimes, the two types of incisions can be combined.
Arm lifting with longitudinal incision along the arm inner side

At first, a lipoaspiration is done, each time fat is found infiltrating the arm region. Then, the skin excess is taking away as necessary, with a longitudinal incision along the arm inner side. The amount and the topography of this skin excess are always located with its limites drawn in collaboration with the patient in a standing position. The average time of the surgery is one hour and half. It may vary, depending on the extent of improvement needed. At the end of surgery, a compressive dressing is done.
This type of arm lifting technique corrects with efficiency the as unsightly as embarrassing skin and fat excess but leaving a scar at the inner side of the arm. This scar often remains visible; it's why a specially rigorous selection of the surgical indications and a perfect patient information and consent are needed.
Considering the disadvantages of this type of arm lifting, from a scar point of view, we try to propose, as often as possible, a less ambitious surgery but with more acceptable scar: as an arm lifting with an isolated armpit incision or a combined procedure with an armpit incision plus a short vertical one of less than 10 cm.
Arm lifting with horizontal armpit incision

The average time of surgery is one hour. At the end of surgery, a compressive dressing is done. Because this procedure is lighter than the previous one, we can do it, most of the time, as day care, under local anaesthetic or under "vigil" one. Such a surgical procedure is certainly less ambitious than the previous one but the main interest of it is its simplicity and lightness, allowing to possibly redo it, one or two times within a few years. The repetition of this procedure will allow, each time, to still improve the result (following the patient wishes) due to complementary skin resection and redraping without elonging the scar which should stay inside the armpit.
Combined technique
This is a synthesis of both previous procedures, realizing a compromising either concerning the advantages or the disadvantages particulary from the scar point of view. This technique combines an horizontal incision inside the armpit with a short vertical one of less than 10 cm, at the arm inner side.
The surgical follow-up
The hospital outing usually takes place the same day or the day after surgery. During the early follow-up period, ecchymosis (bruises) and edema (swelling) can appear. They will decrease within 10 to 20 days after surgery. The pains are normally less important, limited to a certain discomfort, well balanced by the usual pain-killers. The healing period can be a little unpleasant due to the skin tension around the scar borders. So, during this period we must avoid any brusque stretching motion. The necessity to stop working will depend on the type of the professionnal activity. A sedentary work, in most of the cases, can be done again quickly, within a few days after surgery. A sport activity or working out can be done, progressively, again within 4 weeks after surgery. The scar is often pink-red during the first 3 months following surgery; after then it usually decreases progressively during 1 to 2 years. This evololution depends on the patient own skin specificity. During the first 3 months following surgery, the scar must be protected from the sun and UV beams, by using sun blocks.
The result
It will be appreciated within 6 to 12 months after surgery. Most of the time, we can see a good correction of fat infiltration and skin laxity, what improves a lot the arm aspect. The functionnal improvement is also very clear, especially in case of longitudinal incision arm lifting. The scars are usually visible, particulary the longitudinal one, along the arm inner side which is not hidden in a natural fold. Thanks to the technical improvement and to the acquired experience, theresults of this surgery are getting better. It remains, nevertheless, a delicate surgery and even a high rigorous technique never totally protects from a certain amount of imperfections or complications.
Disappointing results
Most of the time, a well-indicated and a well-done inner arm lifting gives a real help to the patient with a satisfactory and expected result. However, localized imperfections are not rare and can be seen, without speaking of complication:
- These imperfections could concern the scar. It can be too visible, stretched or sticked. In case of a too high tension on the sutures, the scar can get an unpleasant aspect (hyper- pigmentation, thickness, retraction, adherence or enlargement). We must know, the scars decrease with time but never deappear totally. Considering this, just remine that it is the surgeon who does the sutures and the patient, the scar. So the scars always follow hazards of scarring process, with a risk of getting hypertrophic requiring a specific treatment. " Concerning the results of the lipoaspiration, they may show either a insufficiency of correction, a slight residual asymetry or small irregularities of the skin.
- These imperfections into the result usually can be treated by complementary beneficial surgery, so called "slight surgical touching up", done under pure local or deepened local anaesthesia. But, no secondary surgery must be done before 6 month post-operatively, where the result starts being stabilized.
Possible complications
Even if it is done for aesthetical purpose, the inner arm lifting remains a true surgical procedure, what means, it can induce the same risks as any surgery as little it is. We must distinguish the complications from anaesthesia and the one from surgery.
- Concerning anaesthesia, it's the anaesthesiologist, himself, who will inform the patient of specific risks. We must know, that the anaesthesia may induce inside the body unpredictables reactions, more or less easy to control : dealing with a competent anaesthesiologist, working in a real surgical environment , pushes down statistically the risks up to an almost insignifiant level. The today techniques offer the patient an optimal security, especially since the patient is in good health.
- Concerning surgery, by choosing a qualify competent plastic surgeon, well trained for this type of surgery, you limit as much as possible all the risks without totally eliminating them however.Complications could always occur after an arm inner side lifting which remains one of the more delicate procedure in the field of aesthetic plastic surgery.
Among, the considering complications, we can quote:
- The general complications : the thrombo-embolic failures (phlebitis, pulmonary embolism) are quite rare but very fearful. Rigorous preventive care must low it's incidence, like, wearing copressive stockings, early raising up or sometimes by using anticoagulant drugs.
- The local complications : the occurence of an haematoma is quite rare but could indicate its evacuation to protect the quality of the aesthetic result / the ocurrence of an infection is furthered by the priximity of a natural fold (usual bacterial pool), we can prevent by a meticulous hygienic care during either the pre- and post-operative period, up to the time of a complete healing.If necessary, surgical drainage and antibiotics can be required. We must know, that infection can leave unaesthetical sequels. / the occurence of persistant lymphatic flow may be seen. It can reach the point of an effusion (swolling), which can necessitate ponctions but in most of the time, will spontaneously desappear without sequels. / Skin necrosis can exceptionally be seen. It is usually limited and localized. To prevent these necrosis, the arm lifting must be well-indicated and the surgery well-adapted and carefully done. / Sensitivity troubles, especially along the inner side of the arm can be seen. Normal sensitivity, most of the time, reappears within 3 to 6 months after surgery.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
As soon as the first liposuction techniques were invented Plastic Surgeons realised that the fat extracted could be re-injected elsewhere in the body, thus acting as a filler. This technique, autologous fat injection, known as lipo-filling, remained disappointing for many years: the re-injected fat tended to be reabsorbed to a great extent, leaving a result, which was neither predictable nor lasting.
Nevertheless Plastic Surgeons were not discouraged and tried to understand the reason for these unsatisfactory results. Little by little progress was made and it was from 1995 onward that the injection of autologous fat became a reliable technique. (S. COLEMAN). The principle is an autograft of fat cells from fat harvested from the patient. Lipostructure can be used for many depressions (troughs) which can be natural or post-traumatic. The aims and indications of this procedure can be summed up as follows:
- Aesthetic indications
- The filling and smoothing of certain wrinkles, especially of the face.
- Restoration of the 'fullness' of a gaunt face or one showing the first signs of aging.
- Restoration of volume and shape to the face : especially in the case of a face emaciated by aging.
- In complement to certain neck- and face-lifts to give a more balanced result.
- As an additional procedure after a previous face-lift, to improve the shape of the mid-section of the face without resorting to another face-lift.
- Indications concerning restorative or reconstructive surgery
- Filling of a depressed zone resulting from injury
- Correction of irregularities following an unsatisfactory liposuction procedure.
- Correction of wasting after triple therapy for HIV + patients.
It is important to keep in mind that lipostructure is a truly surgical technique which must be carried out by a competent, qualified Plastic Surgeon, who is experienced in this technique and who operates in a surgical environment.
Before the operation
Prior to the operation a thorough clinical and photographic examination will have been carried out in order to determine the corrections required. If lipostructure is being used to reduce age-related effects photographs of the patient when young will have been studied in order to analyse the aging process.
- A preoperative check up will be carried out as prescribed.
- An anesthesiologist will see you in consultation at the latest 48 hours before the operation.
- No aspirin-based medication should be taken during the 10 days preceding the operation.
- For certain types of anesthesia you may be required to fast (neither eat nor drink) for six hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
Local anesthesia with sedation given by intravenous drip ('twilight' anesthesia) is the usual choice for lipostructure. One can also use local anesthesia alone, or general anesthesia. The type of anesthesia will be chosen after discussion between yourself, the surgeon and the anesthesiologist.
Hospital stay
The procedure may be carried out on an outpatient basis, in an ambulatory facility, the patient arrives and leaves on the same day. Admission is one hour before surgery, with no food or drink taken for 6 hours before arrival. The patient is discharged three to five hours after the procedure.
The procedure

Each surgeon has adopted his or her own specific technique which he or she adapts in order to obtain the best results in each case. We can however give you some basic points.
We start by carefully defining the areas from which the fat will be harvested, and the re-injection sites. The harvesting of fat is carried out atraumatically through a tiny incision hidden in the natural skin creases, using a small canula. An area with reserves, or even an excess, of fat will be chosen for harvesting, at a site not normally visible.
After harvesting, centrifugation will be carried out for a few minutes, in order to separate the intact fat cells, which will form the graft, from elements which cannot be used. Re-injection is carried out through 1mm incisions using micro-canulas. Tiny particles of fat are re-injected at different levels and in multiple divergent directions. This increases the surface area in contact with the implanted cells and receptor tissue and ensures the survival of the grafted fat cells.
Since there is true bonding of living cells, when the technique is correct and the graft takes, these grafted cells will become a living part of the body. This means that lipostructure is a permanent technique since the grafted fat cells will live for as long as the surrounding tissues.
The length of the procedure varies according to the amount of fat to be re-injected and the number of treated sites. It can vary from 30 minutes to 2 hours for lipostructure alone.
After the operation
After the operation pain is usually mild. Swelling appears during the 48 hours following the procedure; this usually takes 5 to 15 days to disappear completely. Bruising appears after a few hours on the injection sites: it disappears 10 to 20 days after the procedure. Although recovery is in general rapid because of the nature of the procedure, you will have to take into account the swelling and bruising, and organize your social and professional life in consequence. Exposure to sunlight or UV rays must be avoided for the areas concerned for at least 4 weeks otherwise permanent pigmentation can occur. Once the swelling and bruising have settled the final result will begin to be visible 2 to 3 weeks after the procedure.
The result
The final aspect will not be visible before 3 to 6 months. This is usually satisfactory, whenever the indication and the technique have been correct: the depressions have been filled and volume restored. If the graft has taken correctly, we have already seen that the cells remain alive for as long as the surrounding tissues. Nevertheless the result will deteriorate little by little as these tissues age.
Disappointing results
We have seen already that lipostructure, when correctly indicated and carried out, can be beneficial to patients, giving a satisfactory result corresponding to what was expected.
In some cases localized imperfections can be observed (without being true complications): hypo-correction of some areas, slight asymmetry, irregularities. They can usually be corrected by 'touchup' lipostructure under local anesthetic 6 months after the initial procedure, you will have been informed about this possibility.
Possible complications
Lipostructure, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
We must distinguish here between risks related to anesthesia and those related to surgery.
- For anesthesia, the anesthesiologist will explain the risks during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control: the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible. In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the operation is not an emergency and the patient is in good general health.
- Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks, without however eliminating them completely.
Fortunately, real complications are rare following lipostructure which has been carried out correctly. Rounded canulas do not harm the skin, the blood vessels and the nerves In fact practically all the operations go well and patients are completely satisfied with the result.
Infection is normally prevented by prescription of antibiotics before and after the procedure. The most frequent complication of lipostructure is hyper-correction, this is caused by re-injection of an excessive quantity of fat giving an unsightly result. This hypercorrection rapidly becomes permanent and cannot be treated by simple lipoaspiration: it can only be remedied by a true surgical operation to remove the excess fat.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
'Blepharoplasties' means aesthetic surgical procedures of the eyelids aiming to correct unsightly aspects, whether due to heredity or age. They can be performed on the upper or lower eyelids alone, or all four at the same time.
This technique may be carried out alone or in association with other cosmetic facial surgery (brow-lift, forehead-lift, face- and neck-lift) or with techniques such as laser resurfacing, dermabrasion or chemical peels. These procedures can be carried out during the same operation or in two stages.
The goal of a blepharoplasty is to correct signs of aging and remove the tired look due to the heavy eyelids by a more rested, relaxed appearance.
The unsightly aspects most commonly found are the following:
- Drooping heavy upper eyelids, with a more or less marked skin-fold.
- Lower eyelids which have drooped and shrunk, leading to horizontal wrinkles due to distended skin.
- Bulging fat, responsible for 'bags under the eyes' at the lower eyelid level, or sagging upper eyelids
The procedure aims to correct these problems durably by surgical removal of excess skin, fat and muscle, without of course affecting the normal functions of the eyelids. It should be noted that other age-related problems may be present but their treatment necessitates techniques more complex than standard blepharoplasty, or requires supplementary surgery. These problems include sagging of the eyebrows, forehead wrinkles, frown lines, crow's feet at the corners of the eyes, dark rings under the eyes, 'hollow' eyes, 'sad' eyes with down-turned corners, and also skin blemishes and minor scars.
This procedure, for both men and women, is often carried out around the age of forty. It can however be done much earlier where the problem is congenital rather than age-related, for example in the case of bags under the eyes.
Before the operation
Prior to the operation a thorough examination of the eyes and eyelids will have been carried out in order to detect any anomalies which could complicate the procedure or indeed show that it is not recommended in this specific case.
- A specialised ophthalmologic examination will often be prescribed to rule out any ocular pathology.
- A preoperative check up will be carried out as prescribed.
- An anesthesiologist will see you in consultation at the latest 48 hours before the operation.
- No aspirin-based medication should be taken during the 10 days preceding the operation.
- For certain types of anesthesia you may be required to fast (neither eat nor drink) for six hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
Three possibilities exist:
- Local anesthesia alone, in this case the eyelids are numbed by an injection given locally.
- Local anesthesia with sedation given by intravenous drip.('twilight' anesthesia)
- Standard general anesthesia, you sleep throughout the procedure.
The type of anesthesia will be chosen after discussion between yourself, the surgeon and the anesthesiologist.
Hospital stay
The procedure may be carried out on an out-patient basis, in an ambulatory facility, the patient leaves on the same day after a few hours under observation. However, in some cases a short hospital stay can be preferable. The patient arrives in the morning (or sometimes the previous evening) and is discharged the following morning.
The procedure
Each surgeon has adopted his or her own specific technique which he or she adapts in order to obtain the best results in each case. We can however give some basic points.
- Incisions
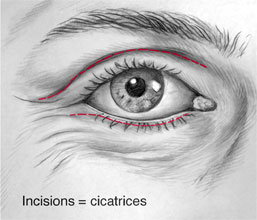
- Upper eyelids: They are concealed in the fold situated at the mid-point of the eyelid, between the mobile and fixed parts.
- Lower eyelids: They are 1 to 2mm below the eyelashes, and can go slightly beyond them.
Note
For the lower eyelids, in the case of isolated "bags" (without excess skin to be removed), a blepharoplasty can be carried out by the transconjunctival approach, that is by using incisions placed inside the eyelids, thus leaving no visible scar. - Upper eyelids: They are concealed in the fold situated at the mid-point of the eyelid, between the mobile and fixed parts.
- Resection
Once the incision made, unsightly excess fat is removed, as are redundant muscle and sagging skin. At this stage, numerous appropriate adjustments can be made in order to tailor the procedure to the specific needs of the patient. - Sutures
Stitches are made using very fine nonabsorbable thread (they are removed a few days after the procedure).
The operation can take between 30 minutes and 2 hours depending on the specific requirements and complexity of the case.
After the operation
There is no actual pain, but possibly some discomfort with a sensation of tension in the eyelids, slight irritation of the eyes and perhaps some blurring of vision. During the first few days rest is advised, with no physical strain, no lifting heavy weights for example. During the recovery period there will be edema (swelling), and bruising, to a variable degree for each individual patient. For the first few days it may be impossible to close the eyes completely, a slight detachment of the external angle of the eye may also be observed, but in both cases these signs are rapidly reversible. The sutures will be removed between the 3rd and 6th day after surgery.
Visible signs of the operation will diminish little by little, a return to normal social and professional activities will be possible after 6 to 20 days. The scars may remain as pinkish lines for the first few weeks, but can be hidden by makeup from the 7th day onward. Slight hardening of the detached zones may persist for a few months, but is not perceptible to others.
The result
The final aspect will not be visible before 3 to 6 months. This is the time lapse necessary for the tissues to regain their softness and for the scars to heal and practically disappear. In general the procedure will have corrected redundant skin folds and removed fatty pads thus rectifying the old, tired look. The results of this procedure are usually among the most durable found in aesthetic surgery. Once the fatty pads removed they do not in general return, so this is a permanent effect. On the other hand skin does continue to age and the excess folds of the eyelids can, over time, recur. However a second operation is rarely envisaged within twelve years.
Disappointing results
These can result from a misunderstanding concerning what can reasonably be achieved. For example lowering of the forehead and eyebrows can only be corrected by a forehead- and brow-lift. They can also be due to unexpected tissue reaction or unusual scarring phenomena. Very fine lines may persist, the eyes may appear slightly too 'hollow' (the bony outline of the eye-socket being visible). Other imperfect results could be a slight downward retraction of the lower eyelids, slight asymmetry, or 'whitish' scars. These imperfections can be remedied by corrective surgery if necessary, usually under local anesthesia from the 6th month following surgery.
Possible complications
A blepharoplasty, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
We must distinguish here between risks related to anesthesia and those related to surgery.
- For anesthesia, the risks will be explained by the anesthesiologist during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control : the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible. In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the operation is not an emergency and the patient is in good general health.
- Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks, without however eliminating them completely.
Fortunately, real complications are rare following a blepharoplasty which has been carried out correctly. In fact practically all the operations go well and patients are completely satisfied with the result.
In spite of the fact that complications are so rare you must be aware of the following possible problems:
- Hematomas: not usually serious, they can be drained if necessary.
- Infections: extremely rare for this procedure, micro-abscesses can develop on stitches but are easily treated. Conjunctivitis will be prevented by routine prescription of eye-drops for the first few days after the procedure.
- Abnormal scarring: this is very rare for the eyelids where the skin usually heals leaving almost no trace of surgery, the scars can however sometimes be more pronounced than hoped.
- Epidermal cysts: they can appear along the scars, but often clear spontaneously, if not they can easily be removed and do not affect the final result.
- Lacrymal problems: excessive tear production is a rarer problem than 'dry eye syndrome' which can decompensate a pre-existing lack of tear production.
- Ptosis: (Drooping of the upper eyelid) : this is very rare except in the over 70's where a pre-existing problem can be made worse by the operation.
- Lagophthalmos: (inability to close the upper eyelid completely) : this can occur for the first few days after surgery but should not persist after a few weeks.
- Ectropion: (lower eyelid retraction) : the severe form is extremely rare following this procedure when it is carried out correctly. The minor form can occur when lax tissue is affected by excessive scar retraction; it usually recedes after several weeks of regular massage which improves the tonus of the eyelids.
- Finally, extremely rare cases of diplopia (double vision), glaucoma, and even blindness following blepharoplasty have been described in International Medical Journals.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
Breast ptosis is the weighing of the breast gland causing a stretching of the surrounding skin and a global sagging of the breast. The breast lies in a too low position and is flattened in its upper part. Breast ptosis can be present from the start, or appear after weight loss or preagnancy with breast feeding. It can be isolated (pure ptosis) or associated to mammar hypertrophy. Conversely, there can be a ptosis with a small breast (hypoplasia or hypotrophic). These aesthetic defaults cannot be paid by your health insurance.
The aim of this operation is to elevate the nipple and areola to a more youthful position, tighten the gland and remove excess skin, in order to obtain lifted and harmoniously shaped breast.
The operation shapes the breast by stretching the skin envelope and concentrating the glandular tissue. The gland is concentrated and put back in proper position, after removal of the skin excess, thus placing the nipple and areola back in a youthful position. The skin incisions are sutured and cause scars.
When the ptosis is very severe, the scars have an anchor shape, with a peri-areolar scar between the brown and white skin, a vertical scar from the areola down to the bottom fold of the breast (infra-mammary fold). The length of the horizontal scar is proportional to the severity of the sagging.
When the ptosis is milder, an isolated vertical scar method can be used, thus avoiding the horizontal scar in the bottom fold and leaving only the peri-areolar and vertical scars. In some very mild breast ptosis, it is possible to use a concentric (or doughnut) mastopexy, which leaves only one scar around the areola.
Finally, in case of a too small breast volume (mammar hypoplasia), breast implants can be added, to restore a satisfying breast volume. In this case, it is usually possible to remove the excess skin around the areola and reduce the scar only to a peri-areolar scar.
Mammoplasty may be performed from the end of adolescence, when growth has ended, throughout life. A further pregnancy or breast-feeding are possible, but we advise to wait for a minimum of 6 months after surgery.
Before the operation
- A preoperative check-up is made according to your surgeon's recommendations.
- You will meet the anaesthesiologist in consultation at latest, 48 hours prior to surgery.
- Besides the usual preoperative examinations, your surgeon might ask you to have a mammogram (breast x-ray) or a breast ultra-sonography.
- No medication containing aspirin will be taken for 10 days before surgery.
Type of anesthesia and hospital stay duration
Breast reduction mammaplasty is usually performed under general anaesthesia. You will be asleep through the entire operation. The duration of hospital stay is usually 2 to 3 days.
The procedure
Every surgeon has his or her personal technical habits which he or she adapts to every new case, in order to obtain the best possible results. However, there are common principles:
- All removed tissues are sent to a special laboratory for microscopic examination (histological exam).
- After surgery, you will wear a "bra-like" dressing with elastic bandage.
- Depending on your surgeon and the severity of your ptosis, the operation can last two to three hours.
After the operation
In most cases, postoperative pain is moderate and usually relieved by ordinary pain medication. Swelling (edema), bruising and pain, when lifting arms upwards are common symptoms.
- Your dressing will be removed after 2 days and replaced with a lighter one, resembling a custom made bra.
- You will leave the hospital 1 to 2 days after the operation and attend consultation 2 to 3 days later. You will then be wearing a surgical bra, which size will have been determined in the hospital, prior to your leaving.
- You should wear the surgical bra day and night for at least one month after surgery.
- Your stitches, if not dissolvable, will be removed 8 to 21 days after surgery.
- You should expect 8 to 15 days convalescence before returning to work.
- You are advised to wait for one to two months before practising any sports.
The result
It can be best appreciated one year after the procedure: the breasts are usually harmoniously shaped, symmetrical and have a natural shape. Besides the physical improvement, this operation usually has a positive effect on weight control, exercise, clothing and psychological health. However, before this final outcome, one should be patient, wait for scars to slowly fade, and accept a regular follow-up every 3 months during one year. The operated breast remains natural and sensitive and responds normally to hormonal shifts.
Disappointing results
The main concern is scars, which will be closely looked after by your physician. They can often be red and swollen for 2-3 months. Then, they slowly fade away and with time, become moderately visible. However they can remain widened, clear or conversely, brown. Regarding scars, it must stressed that even though they usually fade away with time, they never completely disappear. If the surgeon controls sutures, scarring is a patient related process. You may also notice a breast asymmetry, regarding volume, height, size or nipple orientation. All these imperfections can be corrected secondarily, after one or two years.
Possible complications
Mastopexy, even if performed for aesthetic reasons, is a genuine surgical procedure, with the consequent risks related to all medical acts, no matter how mild they might appear.
Post-operative care is usually simple after a Mastopexy. However, complications may occur: some are general, inherent to every surgical act, others are local and most commonly occur in very larges breasts.
There are surgical and anaesthetic complications.
- Concerning anaesthesia, the anaesthesiologist will inform you about all the anaesthetic risks. You must be aware that anaesthesia can sometimes cause unpredictable body reactions that can be difficult to control. The presence of an experienced anaesthesiologist, in a surgical environment, means that the risks are statistically practically negligible. In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, offering optimal safety, especially when the operation is elective and the patient is in good general health.
- Concerning surgery : By choosing a competent and qualified Plastic Surgeon, experienced in performing this procedure, you limit but do not entirely eliminate surgical risks.
Fortunately, genuine complications are rare after a properly performed mammoplasty. In fact, the vast majority of operations meet the patient's satisfaction.
Among possible complications, you must be aware of the following:
- Infection can be treated with drainage and antibiotics.
- Blood clots (haematomas) are quiet rare but can occur. They can be evacuated.
- Localised skin or gland necrosis are rare with modern techniques. They can cause delayed healing.
- Numbness of the nipples may be observed. It is usually transient and most patients recover normal nipple feeling after 6 to 18 months.
Most important to consider is the evolution of scars. These may sometimes become hypertrophic or bumpy (cheloid), in a totally unpredictable manner, thus compromising the final aesthetic outcome. Such pathological scars may require long and specific local treatments.
In most cases however, this operation when correctly planned and executed, does offer very satisfying results in terms of comfort and well being, even if scars are inevitable and remain its major drawback.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
Endoscopy (key-hole surgery) has been used for several years for many types of operation. It consists in operating without a large incision, but rather by introducing a tiny camera into the patient, this then sends pictures to a screen and the surgeon works with special instruments guided by the images. This technique makes it possible to minimize operative traumatism and particularly to reduce problems related to scars.
This technique has been adapted for use in cosmetic surgery where it has been found to be particularly useful for the upper third of the face, that is the forehead and temples. This is called an endoscopic forehead lift. This operation has the aim of correcting unsightly aspects of this part of the face, whether hereditary or age-related, by making a few small incisions (1cm) hidden in the hair. The principle is to detach the entire zone, to weaken the muscles responsible for the wrinkles, then to reposition the tissues and secure them with deep stitches. In certain cases it can be possible to work on a lower zone of the face ; on the cheekbones, the cheeks, and the naso-labial fold around the nose and cheek).
An endoscopic forehead lift can be carried out alone, or if necessary, in association with numerous other facial operations such as ; blepharoplasty (eyelid lift), face and neck lift, laserabrasion, chemical peels, botox injections, etc. An endoscopic forehead lift aims to correct age-related problems of the upper face and to replace a 'tired' or 'severe' appearance by a refreshed, relaxed aspect.
The unsightly features most commonly found are as follows:
- Lowering of the forehead with horizontal furrows
- Lowering of the eyebrows with lateral hoods of the upper eyelids
- Vertical scowl lines between the eyes
- Crow's feet at the corners of the eyes
This procedure, for both men and women, can be carried out at the age of 40. It can however be done much earlier when the problems are hereditary and not age-related, such as eyebrows which are too low, scowl wrinkles caused by muscular hyperactivity.
Before the operation
The motives and wishes of the patient will have been analysed. A careful study of the forehead zone and its proportions compared with the rest of the face will have been made.
- A preoperative check up is done as prescribed.
- An anesthesiologist will see you in consultation at the latest 48 hours before the operation.
- No aspirin-based medication should be taken during the 10 days preceding the operation.
- An antiseptic shampoo will be used the evening before, or the morning of the procedure.
- It is very important to neither eat nor drink for six hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
Local anesthesia enhanced by intravenous sedation ('twilight anesthesia'). General anesthetic during which you sleep throughout the procedure. The type of anesthesia will be chosen after discussion between you, the anesthesiologist and the surgeon.
Hospital stay
This procedure can be carried out on an out-patient basis, in an ambulatory facility, the patient leaves on the day of the operation after a few hours under observation. However, in certain cases, a short hospital stay may be preferable. The patient is hospitalized in the morning (or sometimes the previous afternoon) and leaves the following day.
The procedure
Each surgeon has adopted his or her own specific technique which he or she adapts in order to obtain the best results in each case. We can however give you some basic points:
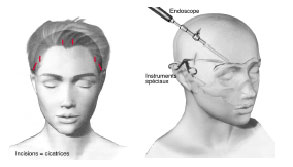
- Skin incisions: There are three to five, they are between 5 and 10mm long and are placed in the scalp a few centimetres beyond the hairline. One of the is for the endoscope which is linked to a tiny camera, the others are for the different instruments specific to this type of surgery. These incisions will of course form the future scars which will be almost invisible since concealed in the hair and also very small.
- Detachment: The entire forehead and temple zone is detached as far as the eyebrows and the bridge of the nose. In some cases this continues as far as the cheekbones and the upper cheeks.
- Muscle weakening: The muscles of this zone are then weakened in order to treat the wrinkles for which they are responsible: the frontalis muscle for the horizontal furrows and the corrugator and procerus muscles for frown lines. Other specific problems can be treated according to the requirements of the case.
- Draping: The detached tissue will be stretched in order to straighten the laughter lines, lift the eyebrows and thus remove the low forehead effect. The tissue is maintained in the correct position by deep stitches of a type determined by each surgeon.
- Sutures: the small incisions are closed, often with easily removed staples.
The procedure lasts between 45 and 90 minutes, depending on the surgeon and the individual corrections required.
After the operation
There is no real pain as such, but a certain tightness around the forehead, the temples and the eyelids. For the first few days you are advised to rest and avoid physical strain. During the post-operative period there will be swelling and bruising which vary in extent and duration for each patient. The dressing will be removed between the first and third day. The clips are removed between the eighth and the fifteenth day. Visible signs of the operation will diminish little by little, a return to normal social and professional activities will be possible after a few days (between 5 and 20 in general). Some numbness of the forehead or sometimes itching of the scalp may occur in the first few weeks. This will gradually disappear.
The result
The final aspect will not be visible before 3 to 6 months. This is the time necessary for the tissues to regain their softness. In general the procedure will have considerably enhanced the appearance of the upper part of the face, giving a younger aspect with raised forehead and eyebrows, tightening of the upper eyelids, removal of crow's feet, and attenuated wrinkles of the forehead and frown lines. This result is in general durable and although ageing is not stopped by the operation, the beneficial result is still visible several years later.
Disappointing results
These can be caused by a misunderstanding concerning what can reasonably be achieved. This is true of wrinkles which may persist in an attenuated form, or excess eyelid skin needing surgical removal for a perfect result. They can also be caused by unexpected tissue changes or unusual scarring. Persistent swelling can occur over some months, or slight asymmetry of the eyebrows, or the return of frown lines. These imperfect results, if perceived as unacceptable can be corrected by 'touch-up' surgery under local anesthetic from the 6th month after surgery.
Possible complications
An endoscopic forehead lift , although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery, however rare they may be, apply here. A distinction should be made between risks related to the anesthesia and those related to the surgery.
- For the anesthesia, the risks will be explained by the anesthesiologist during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions which can be difficult to control : the presence of an experienced anesthesiologist, in a surgical context means that the risks are practically negligible. In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the operation is not an emergency and the patient is in good general health.
- Concerning the surgical aspect : by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks, without however eliminating them completely.
Fortunately, real complications are rare following an endoscopic forehead lift which has been carried out correctly. In fact practically all the operations go well and the patients are completely satisfied with the result.
In spite of the fact that complications are so rare you must be aware of the following possible problems;
- A hematoma: this is not a serious complication but it may be necessary to drain the hematoma if it is large.
- Infection: this is extremely rare when the operation is carried out in a sterile environment.
- Complications such as abnormal scarring, skin death (necrosis) or alopecia (localised hair loss) are rarer and also less marked than with a classic forehead lift since the incisions are reduced in size.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
At present two types of face-lift make it possible to remedy age-related unsightly aspects of the face and neck, either in one area or at a wider level. The face- and neck-lift is the most frequent procedure; this means surgical correction of aging of the neck and also the face from the forehead to the jowls. This cosmetic procedure is not reimbursed by health insurance.
The aim of the operation is to remedy the sagging and laxity of the skin and muscles of the face (forehead, eyebrows, cheeks, jowls, and the oval facial outline) and the neck. The aim here is not only to transform the form and aspect of the face. On the contrary, restoring the different anatomical structures of the face and neck (the skin, the muscles and the fat) enables the patient to look as he or she did some years earlier.
The muscles are tightened, to correct slackness. The skin is then draped as required over the new curves, without excessive stretching. This dual action gives a natural appearance (as the skin is not over-stretched), which lasts (since the muscular base is strong). The healing process is generally uneventful (the skin is less bruised because it is less traumatized, because the tension and separation are limited.) Excess fat, if present can be treated by liposuction.
On the other hand, if the face appears emaciated, this can be corrected at the same time by re-injection of autologous fat. (liposculpture). In this way the face and the neck are 'rebuilt' or 'restructured'. The incisions necessary for the procedure are hidden almost entirely in the hair (at the temples and the nape of the neck) and around the ears. The scar is thus almost entirely concealed.
A face lift can be carried out as soon as signs of aging appear and the patient feels a real need for their correction, generally around the age of 40 or 45. This procedure can be carried out at the same time as another facial cosmetic procedure : blepharoplasty ( for the eyelids), forehead lift (endoscopic forehead lift). It can be completed by other treatment : (laserabrasion, dermabrasion, chemical peels, medical treatment of wrinkles and skin folds, and Botox injections).
Before the operation
Prior to the operation a thorough examination will be carried out as prescribed.
- You will see an anesthesiologist in consultation at the latest 48 hours before the procedure.
- No aspirin-based medication should be taken over the 10 days preceding the operation.
- You must wash your hair the day before the operation and make-up must be thoroughly removed.
- You must fast (neither eat nor drink) for 6 hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
A face-lift can be carried out under general anesthesia or local anesthesia with sedation ('twilight' anesthesia). The type of anesthesia will be chosen after discussion between yourself, the surgeon and the anesthesiologist.
Hospital stay
A 24-48 hour hospital stay is usual.
The procedure
Each surgeon has adopted his or her own specific technique which he or she adapts in order to obtain the best results in each case. We can however give some basic points:
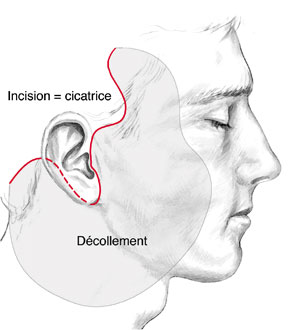
- The incision is almost completely hidden in the hair, or around the ears.
- Once these incisions are made, the skin is detached ; to a greater or lesser extent in each case, according to the degree of sagging of the skin.
- The muscle layer is then carefully and precisely tightened to correct laxity, without affecting the normal expression of the face.
- If there are localized fat deposits, which can form on the neck, the chin, the jowls or the cheeks, lipoaspiration is performed during the operation.
- The skin is then re-draped in a natural manner, excess skin removed, and stitches placed without excess tension.
- Finally a dressing is placed around the head, framing the face.
The procedure lasts from two to three hours depending on the surgeon and the individual corrections required.
After the operation
You will be able to go home on the first or second day after the operation. For the first few days you are advised to rest and avoid physical strain. During this period you should not be surprised by, or worried by, the following:
- edema (swelling) which can be worse on the second day than the first.
- bruising around the neck and chin
- a sensation of painful tightness especially behind the ears, and around the neck.
This bruising and swelling generally disappears in the two weeks following surgery. After one month all signs of swelling have usually practically disappeared. The zones from which the skin was detached may feel slightly hardened, this is perceptible to the touch, but not visible. The ears will not regain normal sensitivity for one or two months. The scars are hidden by the hair both in front and at the back of the head. The only zone where they are visible, in front of the ears, can be temporarily masked by make-up or concealed by the hair.
So, we can say that you are presentable:
- on the seventh day for close friends and family
- on the twelfth day for friends
- after three weeks for people uninformed about the operation.
The result
After two or three months one can have a good idea of the final result. The scars, however will still be slightly pink and hard to the touch, and will not fade until the sixth month after the operation.Through progress over the years and techniques of great precision we usually achieve a result giving an impression of considerable rejuvenation which nevertheless looks quite natural. The face does not have a 'surgical' appearance and has regained the features which it had eight to twelve years before. The general impression is relaxed and refreshed. This physical improvement is also in general psychological. In the long term, a face- and neck-lift has beaten the ravages of time, but aging does continue, and a second similar procedure can be envisaged after about ten years.
Disappointing results
These can be essentially
- edema (swelling) which can persist in certain zones three months after the procedure, and which needs to be treated by massage.
- A partial relapse of sagging skin (ptosis) particularly of the neck, when this was a major problem before surgery.
- Visible scars, or hair loss around the temples (alopecia) which can require revision surgery after six months to a year.
Possible complications
A face lift, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here. We must distinguish here between risks related to the anesthesia and those related to the surgery.
- For the anesthesia, the risks will be explained by the anesthesiologist during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control : the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible. In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the operation is not an emergency and the patient is in good general health.
- Concerning surgery : by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks, without however eliminating them completely.
Fortunately, real complications are rare following a face- and neck-lift which has been carried out correctly. In fact practically all the operations go well and patients are completely satisfied with the result.
In spite of the fact that complications are so rare you must be aware of the following possible problems :
- A hematoma : this must be rapidly drained.
- Infection : This is extremely rare when the procedure is carried out in a sterile environment
- Skin death (necrosis) : this delays the healing process.
- Nerve damage : in particular damage to a branch of the facial nerve, this can lead to paresis, or facial paralysis. This is rare and the after-effects usually disappear in a few months.
- Abnormal scars, either hypertrophic or keloidal : they are impossible to foresee, and their development is unpredictable. They can threaten the aesthetic result and require specific local treatment over a long period.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
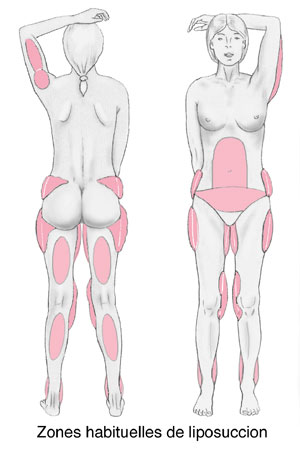
Liposuction can radically and definitively diminish localized areas of protruding fat. These localized areas of protruding fat do not go away with strict diet and exercise. Conversely, liposuction is not a method for losing or controlling weight. Thus, a properly performed liposuction will not replace an improvement in lifestyle. Liposuction is not a treatment for obesity.
The principle of liposuction (as presented in 1977 by Yves-Gérard ILLOUZ) is to remove fat through very small skin incisions, with atraumatic and blunt-tipped cannulas. These cannulas are attached to a closed negative pressure system, which permits safe and sterile aspiration of excessive fat cells. Practically, liposuction can be applied to numerous body areas: hips, outer thighs, abdomen, knees, calves, ankles and upper arms. Technical improvements have permitted to extend its action to the face and neck (i.e, double chin and face oval).
Recent progress in the field of superficial liposuction, performed with very thin cannulas have reduced skin trauma or bruising. It has even improved the final result by enhancing skin shrinkage, when performed with great attention and skill. Meanwhile, it must be kept in mind that liposuction, however common a procedure it has become, remains a genuine surgical intervention, that ought to be performed by a skilled and qualified Plastic Surgeon, specially trained for this technique, in a truly surgical environment.
Before the operation
A preoperative check-up is made following your surgeon's recommendations. The anaesthesiologist will be seen in consultation at latest, 48 hours prior to surgery. No medication containing aspirin will be taken for 10 days before surgery. According to the type of anaesthesia chosen, you may be asked not eat or drink for 6 hours before surgery.
Type of anesthesia and hospital stay duration
Type of anesthesia
Liposuction can be performed, depending on the amount of areas to be treated, either under local anaesthesia, local anaesthesia associated with intravenous sedation or general anaesthesia. In some cases, regional anaesthetics, such as an epidural. The type of anaesthesia will be chosen after a discussion between yourself, your surgeon and your anaesthesiologist.
Hospital stay
The duration of hospitalisation depends on the amount of fat removed. It can be short (a few hours) for small liposuctions under local anaesthesia, or longer (1 or 2 days) for larger liposuctions under general anaesthesia.
The procedure
Every surgeon has his or her personal technical habits which he or she adapts to every new case, in order to obtain the best possible results. However, there are common principles:
- Skin incisions are small (3 to 4 millimeters) and discrete, usually hidden in a natural fold. Fat cells from deep and superficial fat layers are aspirated through smooth cannulas tunneled though subcutaneous tissue layers, taking care to avoid nerves and blood vessels.
- The amount of fat removed is adapted to the amount of the overlying skin, which represents a fundamental factor for the quality of the final result.
- Post-operatively, a pressure dressing is made with an elastic bandage. Very often a special pressure garment is put on top of it.
The duration of the procedure depends on the amount of fat removed and on the number of body areas to treat. It can vary from 20 minutes to 3 hours (average time is 1 to 2 hours).
After the operation
The necessary time needed to recover from surgery is proportional to the amount of excess fat removed. After surgery, you will observe swelling and bruising in the treated areas. Pain can vary from one patient to another, but it is usually mild, due to the use of very thin cannulas. Fatigue is common in the first few post-operative days, especially after large liposuctions. You can go back to your usual activity 4 to 7 days after surgery, again depending on the extent of your liposuction and your type of professional activity. Bruising usually disappears 10 to 20 days after surgery.
It is strongly recommended to wear a pressure garment for 2 to 4 weeks. It is possible to start sports again at least 3 weeks after surgery. There is no dramatic improvement of body contour in the first 2 to 3 weeks, because of the tissue swelling (edema) in the operated areas. It is only after 3 weeks and with the resorption of this edema, that results will begin to appear. The skin will retract completely in 3 to 6 months over the new contours and readapt to the new silhouette.
The result
The final result can be best appreciated 6 months after the procedure. It is most satisfactory when the patient selection and technique are properly done, permitting removal of localized fat deposits and producing skin retraction.
Disappointing results
It has already been explained how liposuction, when correctly indicated and performed, can offer a real improvement to patients in terms of satisfying results and conformity to their expectations. In some cases, localized imperfections can be observed, which must be distinguished from genuine complications: insufficient corrections, residual asymmetry, surface irregularities. These can be corrected secondarily under local anaesthesia after 6 months.
Possible complications
Liposuction, even if performed for aesthetic reasons, is a genuine surgical procedure, with the consequent risks related to all medical acts, no matter how mild they might appear. There are surgical and aesthetic complications.
- Concerning anaesthesia, the anaesthesiologist will inform you about all the anaesthetic risks. You must be aware that anaesthesia can sometimes cause unpredictable body reactions that can be difficult to control. The presence of an experienced anaesthesiologist, in a surgical environment, means that the risks are statistically practically negligible. In fact, techniques, products and monitoring methods have progressed considerably over the last twenty years, offering optimal safety, especially when the operation is elective and the patient is in good general health.
- Concerning surgery: by choosing a competent and qualified Plastic Surgeon, experienced in performing this procedure, you limit, but do not entirely eliminate, surgical risks.
Indeed, some complications can occur after abdominoplasty (tummy tuck) which constitutes one of the most extensive and involved procedures in Plastic and Aesthetic Surgery. Among possible complications, you must be aware of the following:
- Thrombo-embolic accidents (blood clot in the veins of the legs, pulmonary embolism) are rare, but can be life-threatening. They can be prevented by strict prophylactic measures, such as standing and walking as soon as possible after surgery, wearing compression stockings, or heparin therapy (low doses of heparin injected under the skin)
- Blood clots (haematomas) are quiet rare but can occur. They can be evacuated to prevent an impairment of the final aesthetic result.
- Infection, though common, can be treated with drainage and antibiotics.
- It is common to notice 8 days after surgery a lymph collection accumulating under the skin. Such a collection can be drained and will dry up rapidly without sequela .
- Localised skin necrosis. Large areas of necrosis is rare. They can be prevented by a proper surgical examination and a cautious and well-executed operation, with moderate tension on sutures.
- Numbness of abdominal skin may be observed, frequently in the lower abdomen. It is usually transient and most patients recover normal skin sensation after 3 to 12 months.
- In some patients with very damaged skin or skin with poor circulation, the healing process may be delayed resulting in conspicuous scars, which may necessitate a second operation.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
Mammary hypoplasia is defined as a breast volume which is insufficiently developed in proportion to the patient's morphology. It can be a pre-existing condition (small breasts from puberty) or appear later, after substantial weight-loss, a pregnancy followed by breast-feeding, or hormonal problems. It can occur alone or be associated with ptosis, that is sagging of the breasts and skin stretching and a lowered areola.
This insufficient breast volume is often a source of physical and psychological distress for the patient who feels she lacks femininity, with also a lack of self confidence and poor self-image which can lead to an inferiority complex. Breast augmentation with implants is the solution to these problems.
The procedure can be carried out at any age above 18, below this age the procedure is not advisable. This is a purely cosmetic procedure and cannot be reimbursed by health insurance; Only rare cases of total absence of breast formation (mammary agenesis) can be partly reimbursed after prior permission.
The implants used at present are composed of a shell and a filler. The shell is always made of silicone rubber, but the filler can vary. The implant is termed 'pre-filled' when the filler was inserted during the manufacturing process (gel and/or saline solution). The different volumes are therefore fixed by the manufacturer. Implants filled with saline solution are filled by the surgeon who can adapt them to the patient to a certain extent during the procedure.
New generation pre-filled Silicone Gel implants
The great majority of implants used in France and elsewhere in the world are pre-filled silicone gel implants. These implants, which have now been used for over 40 years have been proved to be safe and to be the best product for this procedure since they are very close to the consistency of a normal breast. There has been great progress in this domain since the late 1990's, any weak points have been eliminated. At present all implants available in France have been certified as safe by the EU and the French health and safety agency (Afssaps).
They are made of soft silicone gel inside a strong impermeable envelope of silicone rubber which can be rough or smooth. The most important points concerning the new generation of implants, which ensure their safety, are the new improved envelopes and the gel itself.
The shells, which are now stronger, prevent any leakage of gel (which was a cause of capsule formation) and have much greater resistance over time.
Cohesive silicone gel which has a thicker consistency will not spread in case of rupture of the envelope. Added to this increased reliability is the fact that this new generation of silicone implants exists in different shapes, making it possible to adapt them to individual needs. Thus we find, in addition to the classic round implants, anatomic 'teardrop' shapes which can be higher, wider or more pointed.
This diversity of shape, associated with a range of volumes means that the choice of implant can be tailored to the figure and the expectations of the patient.
Other types of implants
The envelopes are always silicone rubber, it is the filler which can be different. At present in France only two alternatives to silicone gel are authorised:
Physiologic saline
This is in fact salt water (which makes up 70% of the human body). These implants can be 'pre-filled' by the manufacturer or 'inflatable', that is, filled by the surgeon during the procedure. Since the filler is a liquid rather than a gel the breasts do not feel natural, the implants can wrinkle, which can be palpable or even visible; They can also deflate suddenly even after a short time.
Hydrogel
This is the latest substance to have been authorized (in 2005) by the French regulatory agency. It is a water-based gel mainly composed of water and a cellulose-based product. This gel, with a more natural consistence than saline solution, can in the same way be absorbed into the body in case of leakage from the shell.
Before the operation
After discussion between the patient and the physicien who will have clearly explained the different options the best choice for each case is agreed on during the preoperative consultation taking into account all the relevant parameters ( height, weight, pregnancies, breast feeding, body shape, body fat, size of the existing breasts, muscle tone..).
After studying these parameters and anatomic features of the patient, the surgeon will determine the plan for the operation. This will also take into account his preferred technique and the expectations of the patient and the positioning of the scars, the type and size of implants, and the position of the implants above or below the muscle.
- A thorough preoperative examination with blood tests will be carried out as prescribed.
- An anesthesiologist will see you in consultation at the latest 48 hours before the operation. In addition to the usual preoperative tests it can be helpful to use medical imagery, (mammography, echography).
- No aspirin-based medication should be taken during the 10 days preceding the operation.
- You will probably be asked not to eat or drink anything for six hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
This is usually classic general anesthesia, you will sleep throughout the operation. Rarely 'twilight' anesthesia is used (local anesthesia with intravenous sedation), this can be discussed with the surgeon and anesthesiologist.
Hospital stay
One day in hospital is usually sufficient. The patient arrives in the morning (or the previous afternoon) and leaves the next day. However the procedure can be carried out in an ambulatory setting, the patient leaves after some hours of medical supervision.
The procedure
Each surgeon has adopted his or her own specific technique, which he or she adapts in order to obtain the best results in each case. We can however give some basic points:
The incisions
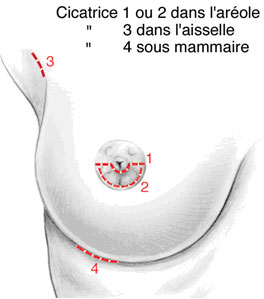
- Peri-areolar approach (around the areola)
The incision is either below the circumference of the nipple or horizontal to the nipple (1&2). - Axillary approach
The implant is inserted through a small incision situated in the armpit (3), or in - The inframammary approach
The incision is in the inframammary fold (4).
These incisions correspond of course to the position of future scars which will thus be hidden in natural folds or lines. Sacars: 1 or 2 in the areola, scar 3 in the armpit, scar 4 in the inframammary fold
The position of the implant
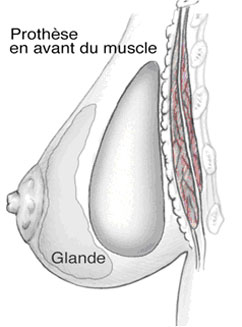
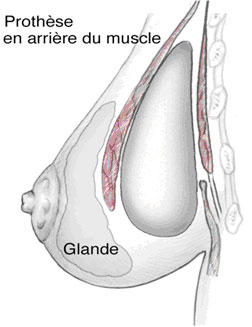
This can be in a pocket made in the breast tissue behind the mammary gland and in front of the pectoral muscle, or behind both the mammary gland and the pectoral muscle. The choice of position will have been predetermined with your surgeon.
- Implant in front of the muscle,
- implant behind the muscle; gland
The choice of position will have been determined in consultation with the surgeon.
Additional surgery
In case of ptosis (sagging breasts, a lowered areola), it is appropriate to associate a breast lift (mastoplexy) ;this implies additional larger scars (around the nipple, or in a vertical position).
Dressings and drains
A drain may be left in place for a few days after the procedure in order to evacuate any blood or liquid which may form around the implant. At the end of the procedure an elastic bra-like bandage is put in place. The length of the procedure varies with each surgeon and of course lasts longer with additional surgery but in general the operation lasts one to two and a half hours.
After the operation
There can be pain for the first few days after the procedure, particularly when the implant is large and/or placed behind the muscle. In this case pain medication of the strenth necessary to dull the pain, is prescribed for several days. Even if there is no pain there will be a strong sensation of tightness. Swelling and bruising of the breasts, and difficulty in raising the arms are frequent immediately after surgery.
The original dressing is removed a few days after the procedure and is replaced by a lighter dressing, then an elasticised bra can be recommended to be worn night and day for a few weeks. If the stitches are non-absorbable they will be removed several days after surgery. Five to 10 days convalescence is necessary before returning to work. Patients are advised to wait for one to two months before practising any sports.
The result
This can be truly seen from two to three months after surgery, the time necessary for the breasts to become softer and for the implants to settle. The procedure will have improved not only the volume but the shape of the breasts. The scars are usually hardly visible. The added breast volume affects the figure in general, this means that more elegant clothes can be worn. Added to this aesthetic improvement there is usually a positive psychological effect due to enhanced femininity.
Duration of results
The implants have their own life-span, (see below) but without taking this into account the result of this procedure concerning volume, is long-lasting. The exception can be when a patient puts on a lot of weight. It is true however the shape and firmness of the 'enlarged' breasts will suffer, like ordinary breasts, from the effects of aging and gravity which cause drooping, more or less rapidly according to age and support quality of the skin, and also the volume of the implants.
Disappointing results
The following problems can occur occasionally:
- Asymmetry of the final volume in spite of the use of different sized implants to correct the problem.
- Stiffness with insufficient softness and mobility (especially with larger implants).
- An artificial appearance especially for very slim patients, the upper limit of the implant is visible.
- The implant can be detected when touched especially when the thickness above the implant is reduced (skin + fat + gland) and when the implant is large.
In cases where the patient is not satisfied with the result certain problems can be corrected by revision surgery after a few months.
Frequently asked questions
Pregnancy/breastfeeding
After having this procedure there is no problem regarding pregnancy either for the mother or the child, but it is advisable to wait for six month safter surgery. Breastfeeding is still possible in most cases.
Auto-immune disease
Many international research papers published on the subject have shown that there is not a higher risk of contracting this type of rare disease with implants compared to the general female population.
Implants and breast cancer
To our knowledge at present we can affirm that breast implants, including those filled with silicone, do not increase the risk of breast cancer. However, during screening techniques clinical examination and palpation can be affected, especially in case of siliconoma or capsular contraction. The presence of the implants can also make it difficult to carry out and read routine mammographies.. It is necessary to explain beforehand that you have implants. Other radiological techniques can be used; echography, MRI etc. Furthermore, if there is doubt as to a diagnosis of breast cancer you must be aware that more invasive exploratory techniques may be used in order to be sure of the result.
How long will the implants last?
Although it is true that some patients can keep their implants for decades without major changes, an implant, whether filled with silicone gel or saline, cannot be said to last for a specific time, this is not a permanent life-long prothesis. A patient with implants must expect them to be replaced at some point in time, if the initial effect is to be maintained. It is impossible to predict the life-span of an implant, of whatever type, as this depends on wear which is variable.
This means that no guarantee can be given regarding their life-span. It should be noted however that the new generation implants are far more hardwearing and reliable. The notion of replacement after ten years is no longer justified, they only need to be replaced if a problem is detected, or the patient wishes to change their size or shape or to correct ptosis.
Follow up
It is important to keep the appointments with your surgeon during the weeks and months following the operation. After this stage regular medical visits with, for example your gynecologist, or for routine mammography will continue this follow up. You must tell each physician that you have breast implants.
A specific visit concerning the implants is advisable every two to three years, but in case of a change observed in a breast, or an accident affecting the breasts, an appointment must be scheduled.
Possible complications
Breast augmentation with implants, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
A distinction should be made between risks related to the anesthesia and those related to the surgery.
- For the anesthesia, the anesthesiologist will explain the risks during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control: the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible. In fact, techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the surgery is elective and the patient is in good general heath.
- Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks to a large extent, without however eliminating them completely.
In general after augmentation mammoplasty the recovery period is straightforward. There can however be complications some of which are inherent to all breast surgery, some linked to the placing of a foreign body in the breast: that is to say risks linked to implants.
- Possible complications inherent to all breast surgery:
A hematoma : blood can surround the implant shortly after surgery. In case of heavy bleeding it is necessary to return to the operating room to drain the blood and put a stop to the bleeding.
Serous effusion : this means an accumulation of lymphatic liquid around the implant. It is a frequent complication often associated with considerable swelling., It gives rise to a temporary increase in the volume of the breast or breasts. It decreases gradually and disappears.
Infection : rare after this procedure. It can require more than one course of antibiotics and the removal of the implant for several months following drainage. After this time interval another implant can be put in place.
Three types of infection exist:
- Late (silent) infection: this has few symptoms and can occur several years after implantation.
- A microabcess: more frequent than the above, they can form on stitches and are absorbed after their removal with local treatment.
- Toxic shock syndrome: rare cases of this have been reported.
Skin necrosis: this occurs when tissue is starved of oxygen due to interruption of blood supply to the zone involved. This can be favored by high blood pressure, hematoma, an infection or heavy smoking by the patient. It is a rare complication but is formidable as, if serious, it can reveal the surface of the implant, notably by splitting the stitches. A second operation is often required, with possibly the need to remove the implant.
Abnormal scar: formation the healing process is unpredictable, and scars can be less discreet than expected. They can be widened, retractile, hyper- or hypo-pigmented, hypertrophic, or rarely, cheloid.
Sensory changes: this is frequently found in the first few months but usually diminishes over time; Rarely however, a certain degree of dysesthesia (heightening or diminution of sensitivity) can persist around the areola and the nipple.
Galactorrhea/milk secretion: very rare cases of unexplained postoperative hormonal stimulation have been reported, giving rise to milk secretion which sometimes collects around the implant.
Pheumothorax : very rare, has specific treatment.
- Specific implant-related risks
Wrinkling or rippling: the implant is soft and natural, and for this reason the outer envelope of the implant can form creases, which can be palpable or visible in certain positions under the skin, giving a 'ripple', effect.
Capsular contractures: it is a normal physiological reaction that a fibrous shell should develop around an implant. A normal reaction to the presence of a foreign body in the organism is to isolate it from the foreign body with a hermetic membrane called a 'periprosthetic capsule'. Normally this membrane is thin, supple and imperceptible but the reaction can increase and the capsule can thicken, become fibrous and contract exerting pressure on the implant, it is then known as a 'capsule' There are four stages of hardening that range from a normal undetectable aspect to severe forms giving hard, round, immobile breasts which can be painful.
Capsular contraction can follow infection or a hematoma, but often has no determined cause, resulting from unpredictable organic reaction. Surgical techniques have made great progress in recent years, but especially the design and products used for the implants are much improved, this means a considerable reduction in the number of cases of capsular contraction and their seriousness. If necessary, he capsule can be incised in a surgical procedure (capsulotomy).
Rupture: we have seen that implants have a limited life-span. An implant can become porous and the silicone rubber envelope of the implant can deteriorate. It can become porous, have tiny leakages or split. This can be rarely after an accident, a puncture with a needle or because of a manufacturing flaw. Much more often, however this is due to deterioration of the implant over time. In all cases this will result in a leakage of the filling product, with different consequences according to the product concerned: If the implant is filled with physiologic solution or resorbable hydrogel the implant will deflate partially or totally, either suddenly or slowly.
With silicone gel (non-resorbable) this will remain inside the membrane surrounding the implant. This can cause capsule formation or can remain un-noticed. In some cases, much rarer now, (mainly because the modern gels are more cohesive), the gel can penetrate the surrounding tissue. Rupture of the implants usually requires an operation to change them.
These are the facts that we wish to bring to your attention in all scientific fairness, concerning augmentation mammography.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
The correction of prominent ears needs a surgical procedure called "otoplasty", which the goal is to reshape the auricles, we think, are excessively too visible. The surgery is usually performed on the two auricles but could be done unilaterally.
An otoplasty corrects the auricle's cartilaginous abnormalities which are the cause of the prominent aspect. Schematically, we can distinguish three types of abnormalities which are often, more or less, associated:
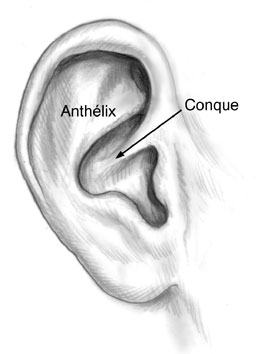
- Too open angle between the auricle and the skull, carrying out the so called "prominence" (valgus helix).
- Too large size of the conchal cartilage (see diagram) projecting forward the ear which improves the prominent aspect (concha hypertrophy).
- Failure into the normal cartilage reliefs folding which gives a too smooth, like "unpleated", aspect to the ear (lack of anthelix plicature).
Surgery, definitively, corrects these abnormalities, by reshaping the ear cartilage, in order to obtain well-positionned, symetrical ears also natural in size and aspect. So, prominent ears surgery also ends the mockeries and other unpleasant remarcks which may have induced psychological difficulties or school problems.
An otoplasty can be performed in an adult, in an teenager or, most of the time in a 6-7 years old child, as soon as the child starts suffering of his/her ear aspect.
Before the operation
A meticulous clinical examination of the ears will be realized by the surgeon himself to determine the needed modifications.
- A usual pre-operative evaluation is done, following the prescriptions.
- An anesthesiologist must be seen in consultation, at least 48 hours before surgery, in case of general anaesthetic or "vigil" one.
- No medicine with aspirin in it must be taken for at least 10 days before surgery.
- Depending on the type of anesthesiology, it can be asked to you to keep fasting (no food, no beverage) for 6 hours before surgery.
- For the boys, a short hair cut is suitable; for the girls, a pony tail is wellcome. But in any patient, the hair must be carefully washed the day before surgery.
Type of anesthesia and hospital stay duration
Type of anesthesia
Three possible proceedings:
- simple local anaesthetic (an analpesic drug is injected locally to insensibilize the ears)
- local anaesthesia completed by tranquillizing drugs, injected in veins ("vigil" anaesthetic)
- classical general anaesthesia, which puts you asleep
The choice between these different techniques must come after you have discussed it with the surgeon and the anaesthesiologist.
Hospital stay
The surgery can be done in the "day care" department; it means, you can leave hospital the same day of the surgery, just after a few hours of resting and medical supervision. On the other hand, you may be asked to stay in hospital over the night; it means, you enter the hospital early morning, the day of surgery (or sometimes the day before in the afternoon) and leave it the day after surgery.
The procedure
Each surgeon is using his own technique, he may adapt to each case, in order to get the best result. But, common surgical steps have to be used:
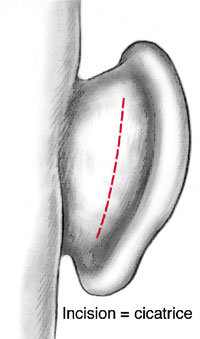
- Skin incisions:
Usually, there are inside the natural retro-auricular fold. But sometimes, some small complementary incisions may take place at the anteror side of the auricles, hidden inside natural folds. Notice that hair will never be cut during surgery.
- Dissection:
The skin will be then undermine to allow the cartilage to be reached.
- Cartilage reshaping:
The principle of this surgery is to create or improve the natural reliefs of the auricles by thinning and/or bending the cartilage framework, which may necessitate deep fine stiches. Sometimes, cartilage cuting or partial removing is indicated. Finally, the auricles are put back in a good position, in relation to the skull, and anchored by deep stiches.
- Sutures: Usually, the skin is closed using absorbable stiches; if not, the stiches must be taken away within 10 days after surgery.
- Dressing:
It is done with elastic bandages around the head to keep the ears in a good position.
Depending on the surgeon and on the gravity of abnormalities to be corrected, the surgery may take half an hour to one hour and half, for both ears correction.
The surgical follow-up
Pains are usually moderate and if necessary, they can be treated using pain killers or anti-inflammatory drugs. In the contrary, in case of persistant pain, you must consult the surgeon or someone of his team. The first big dressing is taking away within 2 to 5 days following surgery. It will be replaced by a lighter one for another few days.
During the early follow-up period, ecchymosis (bruises) and edema (swelling hidding the ear reliefs) can appear. This matter of fact should not worry you; it will be transitory and not affecting the final result. A maintaining and protecting head-band wil be use day and nights for 15 days and then for another few weeks, during night, only. During this period of time, we must avoid any sport activity or working out, especially with risk of contacts. You must also avoid high cold temperature for at least 2 months after surgery, due to the frost-bite risk because of the transitory sensitiveness abatement.
The result
It will be appreciated within 1 to 2 months after surgery. It is the time needed for the edema to disappear, allowing the ear reliefs to be clearly seen. After this period of time, only the scar will be red and harden for another few month before toning down. This surgical procedure will be most of the time efficient to correct auricles abnormalities and to give back natural well positionned, well oriented and well folded ears, also normal in size, symetry and in general aspect.
In most of the cases, the result is definitivelly obtained. But sometimes, a slight (as a rule) recurrence of the prominent aspect of the ear may occur and indicate a slight secondary surgical correction.
To summarize, this quite easy surgery generally allows to efficiently correct unaesthetical prominent ears, ending so the mockeries and other unpleasant remarck which often induce psychological difficulties or school problems.
Disappointing results
They can appear after a while, due to unexpected tissue retraction or unusual scarring process. So, we may, sometimes notice light asymetry between the two ears, small irregularities of the ear reliefs, too acute cartilage plicature, narrowing of the ear meatus or deep stitches feeling.
All these so called "small failures" are discreet and not seen by others. Anyway, we can always correct them and refine the result under local anaesthesia.
Possible complications
Even if it is done for aesthetical purpose, an otoplasty remains a true surgical procedure, what means, it can induce the same risks as any surgery as little it is.
We must distinguish the complications from anaesthesia and the one from surgery.
- Concerning anaesthesia, it's the anaesthesiologist, himself, who will inform the patient of specific risks. We must know, that the anaesthesia may induce inside the body unpredictables reactions, more or less easy to control : dealing with a competent anaesthesiologist, working in a real surgical environment , pushes down statistically the risks up to an almost insignifiant level. The today techniques offer the patient an optimal security, especially since the patient is in good health.
- Concerning surgery, by choosing a qualify competent plastic surgeon, well trained for this type of surgery, you limit as much as possible all the risks however without totally eliminating them. Complications could always occur after an otoplasty but remains quite rare.
Among, the considering complications, we can quote:
- The post-operative bleeding: if it is more then just a blood fleck on the dressing (what should not make you anxious) a esondary surgery may be necessary to stop the bleeding. But the blood, sometimes, can stay inside, giving an haematoma which could indicate its evacuation to protect the quality of the aesthetic result
- An infection is fortunately rare thanks to the rigorous pre-operative asepsis rules. But if an infection occurs, it needs a quick treatment to avoid to reach the cartilage which can have severe consequence.
- Skin necrosis can exceptionally be seen. It is usually limited and localized at the anterior side of ear relief where the skin is very thin and the blood supply disturbed. The scarring just needs local dressings and a small discret scar may remained.
- Abnormal scars: in spite of all the care of the suturing, a ear scar, of any kind, can always become hypertophic or even more "a cheloid scar" the treatment of which remains difficult.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
Rhinoplasty means cosmetic surgery of the nose. This procedure aims to modify the shape of the nasal pyramid (either partially or completely) and can also if necessary correct nasal breathing problems.
A rhinoplasty can be carried out alone or in association with other facial surgery such as a genioplasty (surgery of the chin). This can be done at the same time to modify the facial profile. The aim is to improve the aspect of the nose. The problems present can be congenital, caused by an accident, or due to aging.
The result should be a nose in harmony with the facial features, and which corresponds to the personality and expectations of the patient. The technique uses incisions hidden inside the nostrils and remodels the bone and cartilage which give each nose its distinctive shape. The skin covering these elements will be redraped and will adapt to the new nose. This point shows the importance of the quality of the skin for the final result which is obtained with no visible scar.
When a nasal obstruction impedes breathing it will be treated during the operation. This can be due to a deviated septum (the nasal partition) or hypertrophy of the nasal concha (bony structures inside the nasal cavity). This procedure carried out both for men and women, can be done from the age of 16, when growth is complete.
Before the operation
The motivation and expectations of the patient will have been analysed. Prior to the operation a thorough examination of the nasal pyramid and its harmony with the other features of the face will have been carried with an endo-nasal examination.
- A simulation of the desired result can be done using photos and computer techniques. The virtual image obtained should be considered as a guide to help understand the wishes and expectations of the patient. Nevertheless it should be understood that the final result may be slightly different and not an exact copy.
- A preoperative check up will be carried out as prescribed.
- An anesthesiologist will see you in consultation at the latest 48 hours before the operation.
- No aspirin-based medication should be taken during the 10 days preceding the operation.
- For certain types of anesthesia you must fast (neither eat nor drink) for six hours before the operation.
Type of anesthesia and hospital stay duration
Type of anesthesia
This operation is usually performed under general anesthesia. However, in certain cases local anesthesia with intravenous sedation (twilight anesthesia) may be used. The type of anesthesia will be chosen after discussion between yourself, the surgeon and the anesthesiologist.
Hospital stay
Rhinoplasty is usually carried out in an ambulatory facility, you arrive early at the hospital and are discharged the same day after a few hours under observation. However, in some cases a short hospital stay can be preferable. The patient arrives in the morning (or sometimes the previous evening) and is discharged the following morning, or the following day.
The procedure
Each surgeon has adopted his or her own specific technique which he or she adapts in order to obtain the best results in each case. We can however give some basic points:
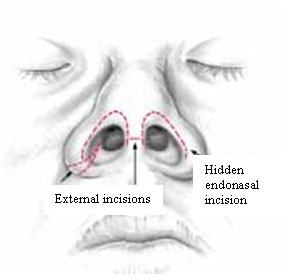
Incisions
As a rule they are invisible, hidden inside the nostrils or under the upper lip, there are therefore no visible scars. It can however be necessary to use an external incision which will be hidden beneath the upper lip. It can be necessary to use an external incision concealed at the base of the nose wings if reducing the nostrils, or across the columna, between the nostrils in order to perform an 'open' rhinoplasty (giving access to the internal structure of the nose. This can be used when repairing serious deformations or for touch-up surgery.
Dissection
These incisions permit separation of the cartilage from the skin and mucosa.
Reshaping the nose
The osteo-cartilaginous structure will then be reshaped as planned. This important step can be carried out in a multitude of ways taking into account the individual case and the preferred technique of the surgeon. The nose may be made smaller or straightened, a bump removed, the tip may be redefined, the septum may be straightened or the nasal concha reduced in size. In some cases a cartilage or bone graft will be used to fill a hollow zone, to support part of the nose or redefine the tip.

Sutures
The incisions are closed with fine sutures, usually dissolving ones.
Dressings and splints
The nostrils are packed with wadding. An external dressing of tape is applied then a splint of plaster, plastic or metal is molded and fixed to the nose, this can sometimes extend to the forehead.
The operation can take between 45 minutes and 2 hours depending on the specific requirements and complexity of the case.
After the operation
There is rarely actual pain, it is rather the fact that the wadding makes it impossible to breathe through the nose which is a problem for the first few days. Swelling can be observed around the eyelids with bruising which is variable in degree and duration for each patient. During the first few days rest is advised, with no physical strain. The wadding is removed 2 to 5 days after the procedure. The splint is removed 5 to 8 days after surgery, to be replaced by a smaller splint for a few more days.
The nose will appear bigger because of swelling and it will still be difficult to breathe because of swelling of the lining of the nose and possible scabs in the nostrils. The visible signs of the operation will disappear gradually and a return to normal social and professional life is possible after 10 to 20 days. Sport and strenuous exercise should be avoided for 3 months.
The result
Two to three months are necessary before the final result becomes appreciable, and it will only be after 6 months to one year that the final aspect will become apparent after a slow and subtle healing process. This result usually corresponds to the expectations of the patient and is fairly close to the initial project drawn up before surgery.
This procedure brings about not only an improvement in appearance which is usually considerable, but also an undeniable psychological benefit. The changes brought about by this operation are permanent. The only modifications which can occur are those which would have occurred in the normal aging process as for a nose without surgery.
Disappointing results
These can result from a misunderstanding concerning what can reasonably be achieved, or be caused by unusual scarring phenomena or unexpected tissue reactions such as poor healing and retractile fibrosis. These imperfections can be remedied by corrective surgery if necessary, usually under local anesthesia from the 6th month following surgery. It is necessary to wait until the healing and scar tissue are stabilised. This touch-up surgery is more simple than the first procedure both regarding the technique used and the postoperative care.
Possible complications
A rhinoplasty, although essentially an aesthetic procedure, is nevertheless an operation, and this implies that the risks inherent to any surgery apply here.
We must distinguish here between risks related to the anesthesia and those related to the surgery. For the anesthesia, the risks will be explained by the anesthesiologist during the preoperative consultation. You must be aware that anesthesia can cause unpredictable reactions, which can be difficult to control : the presence of an experienced anesthesiologist, in a surgical context, means that the risks are statistically practically negligible.
In fact techniques, products and monitoring methods have progressed considerably over the last twenty years, giving optimal safety, especially when the operation is not an emergency and the patient is in good general health.
Concerning surgery: by choosing a competent, qualified Plastic Surgeon, used to performing this procedure, you limit the risks, without however eliminating them completely.
Fortunately, real complications are rare following a rhinoplasty which has been carried out correctly. In fact practically all the operations go well and patients are completely satisfied with the result.
In spite of the fact that complications are so rare you must be aware of the following possible problems:
- Bleeding: this can occur in the first few hours after surgery but is usually moderate. If bleeding persists more wadding should be added, or a return to the operating room may be necessary.
- Hematoma: these must be drained if too painful or too large.
- Infection: in spite of the natural presence of germs in the nostrils this is very rare.
- Abnormal scarring: this can only concern external scars (if any) and is rarely a problem to the point of requiring a second procedure.
- Sores: these are rare but can be caused by the splint. Small sores or wounds heal spontaneously leaving no mark, but skin necrosis, which is very rare, will leave a small scar.
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.
Definition, aims and principles
The botulinic toxin is a substance which decreases the muscle contraction by acting at the level of the neuro-muscular jonction (myorelaxing action).
Since 1975, the physicians are using the botulinic toxin to correct child strabism, facial tics and spontaneous eye blinking. In France, the first official licence ("AMM") dates from 1990 concerning certain pathologies in ophtalmology, ENT, functionnal physiotherapy and neurology.
Concerning aesthetical medicin, Doctor CARRUTHERS, a canadian ophtalmologist, is the first noticing that patients treated with botulinic toxin have less wrinckles around the eye than the others. In 1990, a more observing female patient asked him to balance the other eye : the aesthetical indication is born so.
The botulinic toxin, under the name of "BOTOX" received, in USA, the Food and Drug Administration (FDA) authorization in 2002 for its use to treat the wrinckles in between the two eyebrows.
In February 2003, for the first time, the french administration, in charge of medicine controls, gave an official licence (AMM) for aesthetical purpose to the botulinic toxin, under the name of VISTABEL (Allergan laboratory). This licence concerns the botulinic toxin use for the treatment of the glabella wrinckles under certain conditions of competency from the physician and of using modalities.
If botulinic toxin injections are done outside this anatomical area, they would be done "out AMM". In practice, the more usual indications for botulinic toxin aesthetical injections are the wrinckles between the two eyebrows, the frontal lines and the crow-feet wrinckles. The principle of botulinic toxin consists of using its muscular release properties.
The main goal, we want to reach, is to obtain a decreased muscular action at the level of the forhead and the eyebrows , in order to decrease either the horizontal wrinckles and the vertical ones, done by muscles contraction. Such a use allows to smooth the skin reliefs and so to get a rejuvenative effect due to the muscular tension release. From a more global point of view, we must know that the brow position is fixed by the balance of two opposite forces, one corresponding to lowering muscles (located around the eyebrow) and the other one corresponding to one elevating muscle (the frontalis muscle). The horizontal wrinckles are due to the contraction of the frontalis muscle, and the vertical ones are due to the contraction of the lowering muscles.
This treatment main goal is to improve wrinckles and fine lines, when in a resting position and not to avoid muscle contraction. So, the result will be judge especially on the wrinckles aspect of a quiet face. Concerning the balance between the lowering and elevating muscles, the botulinic toxin, by reducing the action of one muscles group, decrease the wrinckles related to these muscles and free, at the same time, the action the opposed muscles : our aim is to treat the muscular balance, in order to obtain so a facial harmony.
The botulinic toxin treatment must be done and think with time : so, it is recommand, at the time of the first sesion, to treat progressively and to avoid the risk of "doing too much". We should prefer a moderately efficient first session then a too efficient one : so, we don't think, it is suitable to target an optimum as soon as the first injection. In certain cases, it can be necessary to practice several sessions before adapting, for the best, this treatment potentialities, in respect with patient particularities.
Before injecting
No need for special preparation. The day of injection, you don't need to be fasting. For women, it is recommand to come without any make-up or to remove it just before the injection. It is very important to minimize the bleeding risk, at the treated areas, by avoiding aspirin for 15 days before and after the session.
We must also respect the following contra-indications:
- Certain neuromuscular deseases, like myasthenia
- Pregnancy and breast feeding : even if pregnant only for few days pregnancy, you must reschedule the injections after your pregnancy and breast feeding, eventually. So, it is advisable to perform any necessary exam, if you are in doubt and to inform, by giving the results to your physician.
- Known hypersensibility to botulinic neurotoxin A or to serum-albumin
- Present treatment with antibiotics from the aminosid group (Amiklin, Gentallin)
We must also respect a certain number of precautions:
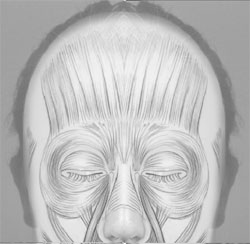
- If you are treated, on the other hand, by botulinic toxin injections, for pathological spasms, if you had an episod of facial paralysis, if you suffer of neuromuscular desease or of cloting failures, you must tell your physician who shoud do your aesthetical botulinic toxin injections. He will judge himself, after contacting your GP, if it is advisable or not to perform these injections and how to do it.
- If before injections, you take medicine, like anti-coagulating drugs or aspirin or antibiotics or if you have any health problem (like infection, flu, dental abcess ...) you must imperatively tell your physician before injections.
- From a general point of view, don't hesitate to mention your physician all even lesser health problem, you had to allow him to see if these injections are advisable. With the same idea, you must tell all your interrogations and mention all the treatments, you.
Type of anesthesia
No anaesthesia is needed.
Injections performance
The tratment is done in the doctor's office or in an hospital, depending on your dostor's choice and habits. This treatment consists on a serie of facial injections. The needle is fine and the injections are usually less painful. The time treatment is a few minutes.
After the operation: the follow-up
During the two hours following the injections, it is advised not doing itense sport and not lying down. It is also advised to avoid facial manipulation or massage for 24 hours following the session. It is very important to minimize the risks of bruises or bleeding at the treated area, for 15 days before and after injections, in order to avoid the injected substance to run away to muscles around what could produce undesirable side effects.
On the other hand, during the three days following injections, it is suitable to strongly contract the injected muscles, three times a day, during about 5 seconds per muscle.
Usually, the after injection is light. Some slightly swollen marks may stay for 20 to 30 minutes before disappearing. The patients can go back to their normal life after the injections. Some rares undesirables but transitory effects may occur like:
- Redness at the injected points, rarely persisting more than 3 to 6 days
- Ecchymosis (bruises), rarely observed and may stay a couple of days
- Edema : a swelling, more often around the eyes, may appear progressively within 4 to 5 days and then decrease within a few days or weeks.
- Sensibility failure : an impression of tension or fixity of the forhead, mouth or neck , depending on the treated area, as well as a modified sensibility, related to the feeling of a "cardboard" skin, may stay for a few days.
- Ocular or facial fugacious pains : such pains have been described in the treated region but remain exceptional.
Whatever, if you have any worry in the post injection period, don't hesitate to contact your physician.
The result
The expected result consists of wrinkles decreasing with small motions keeping; it is obtained within 3 to 15 days following the injections.
Effects: you can see the result after a few days, but for about 15 days, the effects on the face may be variable (even sometimes possibly asymetrical) before ending to stabilize. The result obtained after the first session stays 3 to 6 months averagely, after what the injection can be renewed.
Injection frequency: the injections have to be done several times, with space of 3 to 6 months, before getting a quite stable result. Starting after the second injection, the results may stay longer ( 6 to 8 months). It is then suitable to repeat the injections every 3 to 6 months. But we recommend never reinjecting after a period of time of less than 3 months, to avoid, especially, to cteate a resistance to the substance, due to like "a vaccination effect". The result on the face aspect can be stabilized after 3 sessions but, in certains cases, we may need at least 8 to 10 sessions to get a quite stable result. On the other way, we must remark that if we stop injecting, the treated muscle will go back to its normal function, from before the injections.
Disappointing results
Localized imperfections
In a few cases, some localized imperfections (persistance of small wrinckles) may be seen without speaking of real complication. They depend to the previous aspect of the skin, already marked with deep indelible "fracture" due to the oldness of the wrinckle. It may also exists insufficient or even asymetrical results : they are related to the fact, we have more or less strong muscles and often asymetrical too.
These imperfections are usually treated with a complementary botulinic toxin injection, a month after th injection. Concerning this, we must underline that if a localized complementary injection may be indicated to improve the result, it shouldn't be done before 15 days after the session because the balance between the different muscles takes 15 days to set up.
Residual asymetry
An asymetry between the two sides of the face as well as more marked winckles on side than the other may most often exist before the injection. On the other hand, the muscle responsible of the wrinckle can be stronger on side than on the other.This is generally analysed before the injection. In such a case, the injections will be done in an adapted way, it means, slightly differently on one side compared with the other. Nevertheless, a residual asymetry can persist and eventually profit a complementary injection.
Aesthetical procedures aim to render the patient happier, in a realistic way. But sometimes, we can miss the goal and the procedure may unfortunately improve pre-existing psychological problems. The post-injection experience can extremely different from one patient to the other and this even in case of a comparable aesthetical result.
Concerning botulinic toxin, the rejuvenation is obtained with the contraparty of some facial expression decreasing or even disappearing. This aspect of this treatment would have been evaluated with you to avoid disapointment especialy if you are acting, presenting .....
Possible complications
The complications are very rares. The possible complications are the following:
Facial complications
- Headache: it can appear after the first injections and disappear within a few hours to a few days
- Eyebrow ptosis: frontal injection may produce a slight droping of the eyebrows. This is generally due to a previous low position of the eyebrows. It will usually regress within a few weeks.
- Eyelid ptosis: the injection of the glabella region may induce a partial droping of the upper eyelid which can stay for 4 to 8 weeks. This is quite rare (less than 1% of the cases) and always disappear within a few weeks.
- Smiling and swallowing discomfort: lips injection may induce a smiling discomfort or small abnormal movements. The neck injection may produce swallowing difficulties.
- Eye dryness: due to a decrease tear's secretion, which can produce a keratis, especially on patient wearing contact lens (be aware to well hydrate the cornea)
- Paradoxical muscle contraction and mimic disturbance: in the days following injection, the muscles may present some paradoxical movements (spontaneous contraction) whithout any gravity.
General complications
They are absolutely exceptional.
- Allergic reaction: cutaneous rash, urticaria, general allergic reaction
- Nausea, vertigo
- Tiredness, fever, flu syndrome
- Skin and buccal dryness
All things considered, the risks must not be overestimated, but you must be conscious that an operation, even a minor one, always has some degree of unforeseeable unknown factors. You can be assured that if you are operated on by a qualified Plastic Surgeon, he will have the experience and skill required to avoid these complications, or to treat them successfully if necessary.
These are the facts which we wish to bring to your attention, to complement what you were told during the consultation. Our advice is for you to keep this document and to read it and think it over carefully after your consultation. Once you have done this you will perhaps have further queries, or require additional information. We are at your disposal should you wish to ask questions during your next consultation, or by telephone, or even on the day of the operation, when we will meet in any case, before the anesthesia.

